Beyond the "Stare": Unpacking the Latest in Thyroid Eye Disease Management
- Keshav Narain, M.D.

- Sep 19, 2025
- 5 min read
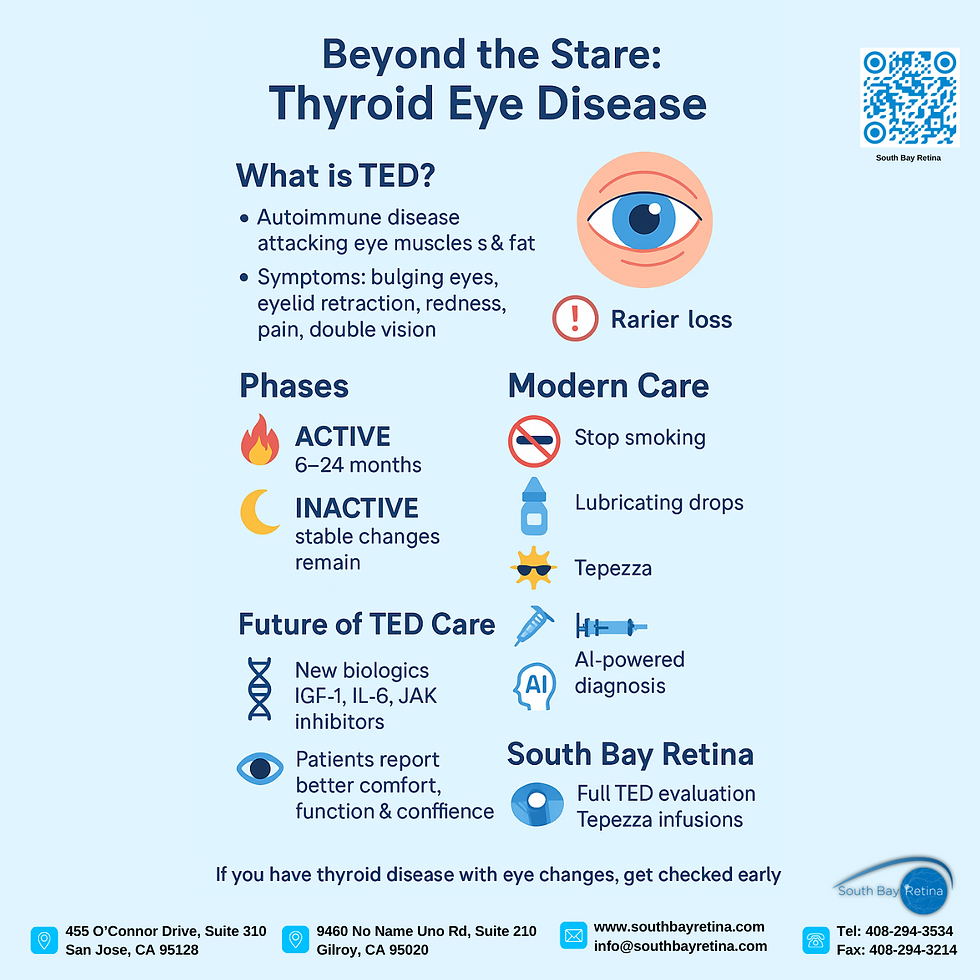
When most people hear about Thyroid Eye Disease (TED), the first thing they picture is that classic “stare”—wide eyes that seem to bulge forward. But TED is far more than just a cosmetic concern. It’s a complex autoimmune condition that can cause irritation, pain, double vision, and, in rare cases, even vision loss. For patients living with it, the challenges go well beyond appearance.
If you or someone you know has been told they might have TED, it’s worth understanding what’s really happening inside the body and what modern treatments can offer.
What Is Thyroid Eye Disease?
TED develops when the immune system mistakenly attacks the muscles and fatty tissue around the eyes. This sets off inflammation and swelling, which can change how the eyes look and feel. Patients may notice their eyes seem to bulge or that their eyelids pull back, creating that “staring” look. Others describe their eyes as gritty, watery, red, or overly sensitive to light. In some cases, the condition causes pain with movement, double vision, or blurry vision that makes daily activities difficult.
The disease usually follows two phases. In the “active” phase, which can last anywhere from six months to two years, inflammation is on the move and symptoms can change quickly. After that, TED settles into an “inactive” phase. The swelling quiets down, but some of the structural changes, like bulging or eyelid retraction, may remain. This timing matters because it guides how doctors approach treatment.
Looking Back: How TED Was Treated in the Past
TED is not new. Physicians as far back as the 19th century noticed the link between thyroid disease and bulging eyes. For much of history, however, treatment options were crude. Surgeons sometimes removed bone from around the eyes to reduce pressure, and later, broad-spectrum steroids or radiation were used. These could calm inflammation but often brought serious side effects. It wasn’t until the 1990s, when TED was fully recognized as an autoimmune condition, that more targeted approaches began to emerge.
Modern Treatment Options
Today, care for TED is far more advanced and collaborative. Endocrinologists and ophthalmologists often work together, because while balancing thyroid hormone levels is important, it doesn’t directly fix the eye disease itself.
Lifestyle plays a major role too. For example, smoking is a well-known trigger that makes TED worse, so quitting is one of the best steps a patient can take. Supportive measures like lubricating drops, wearing wraparound sunglasses, or even sleeping with the head slightly elevated can provide real comfort. In milder cases, studies suggest that selenium supplements may also help.
The biggest breakthrough in recent years is a medication called Tepezza (teprotumumab). Approved by the FDA in 2020, it’s the first therapy developed specifically for TED. Tepezza works by blocking a receptor that drives inflammation in the orbit. In clinical studies, patients had significant improvements: eyes that looked less bulged, double vision that eased, and pain that diminished. For many, it has been a life-changing treatment.
Other treatments still play a role, especially in more severe cases. High-dose steroids are sometimes used during the active phase, though their side effects—weight gain, diabetes, bone loss—require careful monitoring. Orbital radiation may be helpful for select patients. And once TED enters its stable phase, surgery may step in to restore function and appearance, whether by decompressing the orbit to make more space for swollen tissues, adjusting eye muscles to improve double vision, or repairing eyelids that have pulled back.
The Challenges We Still Face
Even with these advances, TED isn’t easy to manage. Doctors continue to debate whether radioactive iodine treatment for Graves’ disease worsens TED, and if so, how to best protect patients. Timing is another gray area: when is the ideal moment for surgery if someone is also receiving new biologic therapies? Then there’s the reality that Tepezza, while effective, is costly and not yet widely available in many parts of the world.
Another often overlooked issue is the emotional toll. Living with TED can affect confidence, self-image, and daily life in profound ways. This is why quality of life—not just clinical results—needs to be at the center of every treatment plan.
The Future of TED Care
Despite the challenges, there’s real hope on the horizon. Researchers are exploring next-generation therapies, including oral and injectable versions of IGF-1 receptor inhibitors, drugs that target IL-6 or JAK pathways, and even antibody-lowering treatments. Some scientists are studying the potential of gene therapy and regenerative medicine, which could one day repair damaged tissue. At the same time, better diagnostic tools and artificial intelligence may soon help doctors predict which patients will benefit most from which treatments. The future is moving toward care that is more precise, more effective, and easier on patients.
Our Experience at South Bay Retina
Here in San Jose, our team at South Bay Retina provides comprehensive diagnostic and treatment services for TED. We start with a full evaluation that includes measurement of eye movement, a complete eye exam, visual field testing, and a highly specialized test called a visual evoked potential. Once we review the results, we sit down with each patient to discuss the options, weighing the pros and cons together.
For those who are candidates, we offer Tepezza infusion therapy in a comfortable clinic setting. Our infusion nurse is highly experienced, and patients often report feeling more at ease knowing they are in good hands. We have seen excellent outcomes—patients not only look and feel better but also notice real improvements in their daily lives.
If you have thyroid disease and are experiencing irritated eyes, redness, bulging, double vision, or pain when moving your eyes, it may be a sign of TED. Not every patient has the same symptoms, but early evaluation makes all the difference.
Closing Thoughts
Thyroid Eye Disease is complex, but with modern treatments and a dedicated care team, patients have more options and more hope than ever before. From supportive measures to cutting-edge therapies, progress is being made every year. The key is early diagnosis, the right specialists, and a personalized approach.
Connect with Us!
You can reach us and learn more through the following channels:
Website: https://www.southbayretina.com
Phone: (408) 294-3534
Proudly serving patients throughout Santa Clara County, including San Jose, Gilroy, and the greater South Bay.
𝗬𝗼𝘂𝗧𝘂𝗯𝗲: youtube.com/@NarainEye
𝗜𝗻𝘀𝘁𝗮𝗴𝗿𝗮𝗺: https://www.instagram.com/south_bay_retina
𝗙𝗮𝗰𝗲𝗯𝗼𝗼𝗸: https://www.facebook.com/narain1
References
Bartalena, L., Kahaly, G. J., Baldeschi, L., Dayan, C. M., Eckstein, A., Marcocci, C., ... & Wiersinga, W. M. (2021). The 2021 European Group on Graves' orbitopathy (EUGOGO) clinical practice guidelines for the medical management of Graves’ orbitopathy. European Journal of Endocrinology, 185(4), G43–G67. https://doi.org/10.1530/EJE-21-0479
Douglas, R. S., Kahaly, G. J., Patel, A., Sile, S., Thompson, E. H. Z., Perdok, R., ... & Smith, T. J. (2020). Teprotumumab for the treatment of active thyroid eye disease. New England Journal of Medicine, 382(4), 341–352. https://doi.org/10.1056/NEJMoa1910434
Smith, T. J., & Hegedüs, L. (2016). Graves' disease. New England Journal of Medicine, 375(16), 1552–1565. https://doi.org/10.1056/NEJMra1510030
Narain, K. (2025). Clinical insights and management strategies for Thyroid Eye Disease. South Bay Retina, San Jose, CA.
WATCH THE FULL VIDEO'S HERE:
LISTEN TO THE PODCAST EPISODE HERE:
.png)



Comments